For further information, access the links listed below. Is your test, item, or service covered? The BCRC does not process claims or claim-specific inquiries. Medicare entitlement.

This single-source development approach greatly reduces the number of duplicate MSP investigations. This also offers a centralize one-stop custo. See full list on cms. For example, information submitted on a medical claim or from other sources may result in an MSP claims investigation that involves the collection of data on other health insurance.
MACs, intermediaries, and carriers will continue to process claims submitted for primary or secondary payment. Claims processing is not a function of the BCRC. If a provider submits a claim on behalf of a beneficiary and there is an indication of MSP, but not sufficient information to disprove the existence of MSP, the claim will be investigated by the BCRC. This investigation will be performed with the provider or supplier that submitted the claim.

The goal of MSP information gathering and investigation is to identify MSP situations quickly and accurat. Information received because of MSP data gathering and investigation is stored on the CWF. MSP data may be update as necessary, based on additional information received from external parties (e.g., beneficiaries, providers, attorneys, third party payers). MSP records that you have identified as invalid are reported to the BCRC for investigation and deletion.
The BCRC’s trained staff will help you with your COB questions. Whether you need a question answered or assistance completing a questionnaire, the Customer Service Representatives are available to provide you with quality service. Click the Contactslink for BCRC contact information. In order to better serve you, please have the following information available when you call: 1. If you cannot furnish a provider number that matches the BCRC’s database, you will be asked to submit your request in writing. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.

Answer your questions concerning how to bill for payment. Process claims for primary or secondary payment. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the trading partners. The COBA Trading Partners document in the Download section below provides a list of automatic crossover trading partners in production, their identification number, and customer contact name and number.
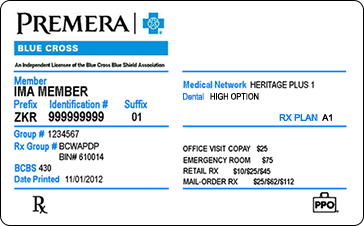
For additional information, click the COBA Trading Partnerslink. To access MLN Matters articles, click on the MLN Matterslink. This list only includes tests, items and services (both covered and non-covered) if coverage is the same no matter where you live. Eligibility and Benefits Our eligibility and benefits tools help you verify member eligibility , determine benefits , view care plans and get digital ID cards. What Would You Like to Do?
Use this chart to learn more about each plan. It also serves as proof that you have applied for benefits or that you have never received Social Security benefits or SSI. You can see plans and associated payer IDs to look up eligibility and benefits information electronically.
Verification of coverage is not a guarantee that payment will be made. It is only a statement of the in-force status of the policy and a description of the maximum benefits that it may provide.