Randomised trials and informed consent. Informed consent is typically seen as most relevant to surgical and other invasive specialties. Although family physicians perform fewer high-risk procedures, they are nonetheless extensively involved in the informed consent process because of the comprehensive and continuing nature of the family physician-patient relationship. The History of the Informed Consent Requirement in United States Federal Policy I. Introduction The informed consent provision in United States federal policy serves a crucial function by protecting human subjects participating in medical research experiments.
This paper will trace the development of informed consent as a legal doctrine. Comment in Med Sci Law. The issue squarely presented in this petition is whether expert medical testimony is required to establish the standard of care of health care providers on the issue of informed consent. For example, a patient may give informed consent to medical treatment only after the health care professional has disclosed all possible risks involved in accepting or rejecting the treatment.
A health care provider or facility may be held responsible for an injury caused by an undisclosed risk. Patients have the right to receive information and ask questions about recommended treatments so that they can make well-considered decisions about care. Successful communication in the patient-physician relationship fosters trust and supports shared decision making. In the USA there is a federal statute applying Informed Consent to medical experiments and IRBs (Institutional Review Boards). Significantly, there is also the UN Declaration on BioEthics, negotiated in Geneva, using.
The obligation to obtain informed consent arises out of respect for persons and a desire to respect the autonomy of the individual deciding whether to volunteer to participate in biomedical or health research. Except in emergencies, healthcare practitioners must generally obtain the patient’s informed consent before providing treatment. If the patient lacks capacity due to age or incompetence, consent must be obtained from a personal representative authorized by law to provide consent. Failure to obtain or properly document informed consent may subject practitioners to civil, administrative.
This written authorization can limit professional liability issues for the individual providing the service. These principles, the court argue were consistent with both a woman’s right to reproductive choice and doctor-patient. The rule leaves untouched many state laws that traditionally govern the doctor-patient relationship.

One of these laws is embodied in what is known as the doctrine of informed consent. What is Informed Consent ? Under the doctrine of informed consent , a doctor must inform a patient as to the risks and benefits of a proposed course of treatment. The Court of Appeals concluded that the trial court erred in submitting the informed consent issue to the jury and reversed and remanded for a new trial. Informed Consent entry and the Encyclopedia of Law are in each case credited as the source of the Informed Consent entry. The department shall promulgate regulations to obtain informed consent and to protect the dignity of the individual.
Autonomy and Informed Consent – issues relevant to Shared Decision Making. Securing informed consent , though vital to any defense, will not shield a practitioner from a malpractice claim. That is because courts generally hold that patients cannot consent to negligent treatment. Burch did notchallenge Florida’s law which stipulated that a candidate for voluntary admission to amental hospital give his “express and informed consent. His contention was thatboth the hospital (and the community mental health center, which was later dropped fromthe suit) had wilfully and wantonly failed to follow the law.

The purpose of obtaining informed consent is to ensure that patients know what doctors propose to do and freely grant their permission. The law has long recognised the principle that every person has the right to have his bodily integrity protected against invasion by others. The seriousness with which the law views any invasion of physical integrity is based on the strong moral conviction that everyone has the right of self determination with regard to his body. A physician has a duty to inform a patient in lay terms of the dangers inherently and potentially involved in a proposed treatment.
It is here that the social meaning of consent becomes most evident. If the individual is capable of providing informed consent, written consent must be provided by the individual and witnessed. Some medications and surgical operations may be able to treat certain health problems.

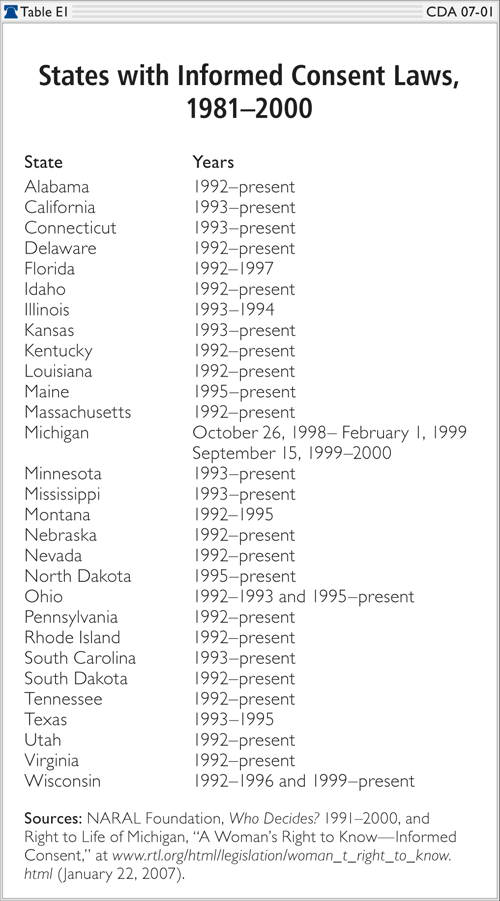
However, the same treatment may also bring some health risks and complications to the patient. Learn more about the laws and process of informed consent. Properly executed informed consent forms for procedures and treatments specified by the medical staff, or by Federal or State law if applicable, to require written patient consent.
Interpretive Guidelines §482.