What is required for an abn? Is an ABN required for Medicare? When to use an advanced beneficiary notice (ABN)? The ABN must describe an extended or repetitive course of noncovered treatment as well as a list of all items and services believed to be non-covered. If applicable, the ABN must also specify the duration of the period of treatment.
A new ABN is required when the specified treatment extends beyond one year.

For an ABN form to be acceptable, it must: 1. See full list on med. Under LOL, a beneficiary can be held liable for a service denied due to reasons cited on the ABN. The financial liability protections (FLP) provisions of the Social Security Act (the Act) protect beneficiaries and health care providers (physicians, practitioners, suppliers, and providers) under certain circumstances from une. If the beneficiary was not properly notified of possible disallowed Medicare claims, the RR state that suppliers must refund any amounts collected. The RR provisions require that a beneficiary is notified and agrees to the financial liability.
Prior to rendering a service in which Medicare may consider not medica. Under the revised ABN instruction, CMS advises that it may be used to voluntarily notify Medicare beneficiaries of an expected noncovered denial of Medicare payment due to the statutory exclusion of an item or service, or the item or service not meeting the definition of any Medicare benefit.
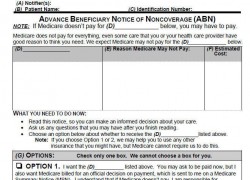
Statutorily Excluded Items or Situations (Not all inclusive) 1. Durable Medical Equipment and r. CMS Beneficiary Notices Initiative (BNI) 3. As part of this process, the notice is subject to public comment and re-approval every years. With the latest PRA submission, a change has been made to the ABN. An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
If the provider does not deliver a valid ABN to the beneficiary when required , the beneficiary cannot be billed for the service and the provider may be held financially liable. Most of us are familiar with the term ABN and have a general idea of when it should be use but there are some. If there are ANY changes, a new ABN is required. Access the below information from this page. Since all patients are on different treatment protocols, there is no reason to automatically require every patient to sign a new ABN at the beginning of each year.
An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered medically necessary. An ABN is used when service(s) provided may not be reimbursed by Medicare. requires your Alabama nursing license number and the last four digits of your social security number as your pin number. If you are required to complete the class, you must view each segment of the class to earn the four () contact hours of continuing education.
It must be issued when the health care provider (including independent laboratories, physicians, practitioners and suppliers) believes that Medicare may not pay for an item or service because of medical necessity, frequency limitations, discontinued services, experimental and investigational, and not.

An advance beneficiary notice ( ABN ) is a written notice which a physician, provider, or supplier give to a Medicare beneficiary before items or services are furnished when the physician, provider, or supplier believes that Medicare probably or certainly will not pay for some or all of the items or services. When a physician or supplier has a “genuine doubt” that a service will be covere they are required to notify the patient of this fact. The ABN form is needed to be used for a statutorily covered service that may not be deemed to be medically necessary.
As such, registering for and acquiring an ABN must take place before your new business begins trading. Advance beneficiary notice of non-coverage. For example, “wound care supplies” would be a sufficient description of a group of items used to provide this care. An itemized list of each supply is generally not required. When a reduction in service occurs, notifiers must provide enough additional information so that the beneficiary understands the nature of the reduction.
Noncoverage ( ABN ) (Form CMS-R-131) for all situations where Medicare payment is expected to be denied. The revised ABN replaces the ABN -G (Form CMS-R-131G), ABN -L. A Signed ABN is Required for This Requisition, and submit the signed ABN, even if you added a diagnosis that the payer considers to be medically necessary.
Include a signed ABN with the requisition: a Click No, File Order. The SREP requirement consists of a Pillar minimum requirement of 4. Pillar requirement, a capital conservation buffer of 2.