
Gillick Competence – Consent to medical treatment for minors An adult of ‘sound mind’ can provide valid consent to medical treatment, including a refusal of treatment that would lead to deterioration in their health, or even death. Can Gillick consent to medical treatment? Children under the age of can consent to their own treatment if they’re believed to have enough intelligence, competence and understanding to fully appreciate what’s involved in their treatment. Otherwise, someone with parental responsibility can consent for them. In some situations children are able to give consent themselves, and sometimes others need to take the decision on their behalf.

This factsheet sets out the basic information to enable you to obtain the appropriate consent from children and young people. See full list on medicalprotection. When caring for children, you have an overriding duty to act in the best interests of the child.
When making decisions regarding treatment, the child or young person should be involved in the decision as much as possible, depending on their level of understanding. Aged and 17A child’s affirmative consent (assent) to investigation or treatment deemed in their best interests, having achieved the age of 1 cannot be overruled by anyone with parental responsibility, although the court may in its capacity a. However, you should consider carefully whether overriding the consent of a distressed child , given the clinical circumstances at the time , is necessary. Often, if sufficient time is given, the parents will be able to encourage the child that the intervention will be beneficial.
You should aim to work in partnership with the parents, assuming that the child’s best. The same principle applies if the parents of a noncompetent child choose to withhold consent for what you believe to be necessary treatment. You are obliged to act in the child’s best interests and these situations, whilst rare, will likely be fraught and legal advice should be sought.
It is important to record any decision made in the patient’s notes. This should include the information that was provided to the patient and the parents and how the decision was reached. Medical Protection factsheet, Access to Medical Records 2. GMC, 0-years: Guidance for all Doctors 3. DH, Consent: A Guide for Children and Young People 4. DH, Seeking Consent: Working with Children. The consent of a person with parental responsibility for the child is required in order to proceed with treatment in any case where that child does not pass the Gillick Test for Competence.
In all cases, there is the ever-present duty of care to keep the child’s best interests at the heart of decisions about their health care. The following information looks at how this can be applied in practice. To a more limited extent, and year-olds can also take medical decisions independently of their parents.
Victoria Gillick challenged Department of Health guidance which enabled doctors to provide contraceptive advice and treatment to girls under without their parents knowing. It was determined that children under can consent if they have sufficient understanding and intelligence to fully understand what is involved in a proposed treatment, including its purpose, nature, likely effects and risks, chances of success and the availability of other options. However, as with adults, this consent is only valid if given voluntarily and not under undue influence or pressure by anyone else. Additionally, a child may have the capacity to consent to some treatments but not others.
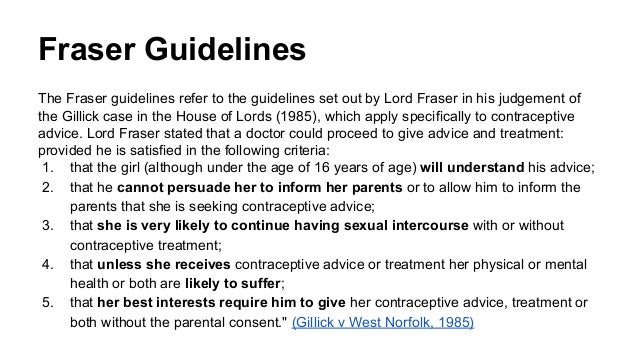
The ‘Fraser guidelines’ specifically relate only to contraception and sexual health. They are named after one of the Lords responsible for the Gillick judgement but who went on to address the specific issue of giving contraceptive advice and treatment to those under without parental consent. The House of Lords concluded that advice can be given in this situation as long as: 1. The advice or treatment is in the young person’s best interests.
That sai it would rarely be appropriate or safe for a child less than years of age to consent to treatment without a parent’s involvement. When it comes to sexual health, those under are not legally able to consent to any sexual activity, and therefore any information that such a person was sexually active would need to be acted on, regardless of the of the Gillick test. However, unlike adults, their refusal of treatment can in some circumstances be overridden by a parent, someone with parental responsibility or a court. This would include circumstances where refusal would likely lead to death, severe permanent injury or irreversible mental or physical harm. If a young person under the age of presents to a health care professional, then discloses a history raising safeguarding concerns: 1. In bothcases, the health professional should inform the young person of this action, unless doing so could pose significant additional risk for their safe care.
It is reasonable for the local authority or police to decide whether it is appropriate to inform the parents of the concerns raised. In some circumstances this may not be in the best interest of the young person. Fraser guidelines are used specifically for children requesting contraceptive or sexual health advice and treatment. However, there is still a duty to keep the child’s best interests at the heart of any decision, and the child or young person should be involved in the decision-making process as far as possible.
Older children (or rather ‘mature minors’) may have sufficient understanding and intelligence to consent to health care treatment themselves. Most – but not all – year old children would not be able to give informed consent to anything much beyond what they would like to eat or what clothes they would like to wear. Victoria Gillick set in motion a series of legal proceedings addressing the issue of consent by minors that continues to guide us today. The routine assessment of competence in under 16s should be appropriate to the child’s age.
Facts Mrs Gillick was a mother of five children, one of whom had sought and received contraceptive advice from a local doctor whilst below the age at which she could lawfully consent to intercourse. This advice was provided pursuant to guidance issued by the Department of Health and Social Security. Gillick competence is the principle we use to judge capacity in children to consent to medical treatment.