Do Not Resuscitate orders? What does do not resuscitate really mean? Do not resuscitate tattoo sparks legal and ethical dilemma? Is a do-not-resuscitate order ever ethical? Sumrall W Mahanna E, Sabharwal V, Marshall T. It’s now gone into effect in hospitals across the state.

While the intent is to protect patient autonomy, it also raises ethical concerns. Sometimes it also prevents other medical interventions. Allow Natural Death (AND) Decisions.
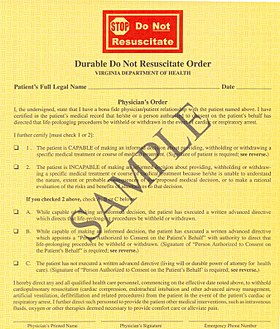
Status: Revised Position Statement. Originated by: ANA Center for Ethics and Human Rights. Adopted by: ANA Board of Directors. A do-not-resuscitate (DNR) order placed in a person’s medical record by a doctor informs the medical staff that cardiopulmonary resuscitation (CPR) should not be attempted. Because CPR is not attempte other resuscitative measures that follow it (such as electric shocks to the heart and artificial respirations by insertion of a breathing tube) will also be avoided.
Ethical debate ‘remains unsettled’. Physicians are evenly divided as to whether unilateral do not resuscitate (DNR) orders — decisions about resuscitation made by doctors without patient or surrogate consent — are appropriate, found a recent study. The debate over this topic in the ethical literature remains unsettle” says lead author Michael S. Putman, M a fellow in the department of medicine at Northwestern University in Chicago.
There are circumstances in which an order not to resuscitate may properly be issued in connection with the care of a patient. Given the diversity of published opinions and cultures within our society, an essential element of preoperative preparation and perioperative care for patients with Do – Not – Resuscitate (DNR) orders or other directives that limit treatment is communication among involved parties. It is necessary to document relevant aspects of this communication. Informed decision-making cannot be. Instant Do wnloa Mail Paper Copy or Hard Copy Delivery, Start and Order Now!
The decision not to resuscitate must be conveyed to all appropriate medical, nursing and other staff. These apprehension s are present because of the uncertainties that lay between the doctors and family for the decision-making authority over the patient. The argument is that patients should die peacefully without undergoing painful and ineffective treatment. As with any end of life decision, there are ethical issues that need to be addressed in order to fully and ethically complete a do-not- resuscitate order. Generally patients must give informed consent before do-not-resuscitate (DNR) orders.
Only of competent patients are involved prior to the dec …. Resuscitating a patient who undergoes a cardiac arrest or stops breathing often involves multiple procedures. Difficulties and confusion about do not resuscitate (DNR) orders still exist, despite efforts to help patients, families, and surrogate decision-makers make informed choices. Instantly Find and Do wnload Legal Forms Drafted by Attorneys for Your State. DNR orders come from physicians, not from patients. However, as technology evolves and the story of Frankenstein reborn with a bolt of lighting has come true with the external or implanted defibrillators, the natural process of death slows as much of society gains the knowledge to live longer than nature intended.

Birtwistle J(1), Nielsen A. Author information: (1)University of Southampton, Department of Psychiatry, Royal South Hants Hospital. The aim of sociological research is to investigate and describe social life, social values and traditions, population and social variables. Such cases would involve patients for whom resuscitative efforts would be ineffective or.
The do-not-resuscitate (DNR) order, a medical and legal document that reflects the patient’s decision and desire to reject life-sustaining interventions, is predicated on the concept that patients (or their surrogates) may choose to forgo certain resuscitative procedures—and their possible benefits—because they reject the possible burdens associated with them. A DNR decision can be a complex process involving nurses and physicians with a wide variety of experiences and perspectives.