Anthony Fauci said he would “definitely not” support a nationwide mandate of the COVID-vaccine. It’s a different story for orders issued by states, cities or businesses, but even then. Australia says it will secure almost million doses of a coronavirus vaccine if two promising. Australians are likely to face mandatory coronavirus vaccinations if Prime Minister Scott Morrison gets his wish.
Can I be really clear to everyone? The Federal Government has announced the end of the conscientious objector exemption for access to the Child Care Rebate, Child Care Benefits and Family Tax Benefit Part A end of year supplement. Australia has some of the strictest vaccination policies in the worl and the No Jab, No Pay scheme has seen a significant increasein national vaccine compliance. Primary Health Network areas achieved an immunisation rate of or more.
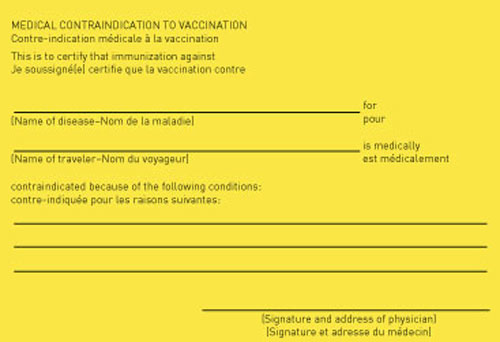
Currently, only three vaccines are mandatory : diphtheria, tetanus, and polio. New laws will stipulate that all childhood vaccinations currently recommended by health authorities will be compulsory. Although the numbers are small, there are good reasons to be concerned about parents who don’t vaccinate their children, or who delay getting their children’s vaccinations. First, the national targetfor vaccination coverage is. Plateauing at isn’t good enough: more needs to be done.
Secon the parents who reject vaccines tend to cluster in certain regions. This can result in small communities having very low vaccine coverage. In these communities babies who are too young to be vaccinate older people whose immunity has wane and people whose immune systems are compromised by a medical condition are more vulnerable during outbreaks. Children who aren’t fully vaccinated are not protected if there is an outbreak of disease.
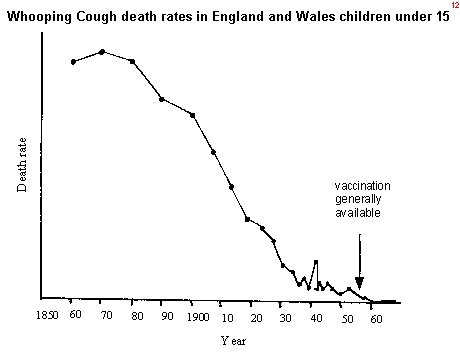
Outbreaks of measles, meningococcal disease, and whooping cough capture wide public attention because they spread easily and can cause very serious illness. However the current childhood vaccination scheduleis designed to prevent at least diseases, and. See full list on theconversation.
Vaccine scares, whether rumours or theories about vaccines being harmful, or genuine safety issues, can undermine parents’ confidence in the safety of vaccination. When parents who are scared turn to other parents (in their social networks, or through social media) for reassurance, they often encounter people who are convinced vaccines are unsafe, or that it is safer to avoid vaccination. The ripple effects from this scare, which has repeatedly been shown to be unfounde continue to undermine parents’ confidence in vaccines around the world. We suspect the reason there is so much talk about parents who choose not to vaccinate is because we don’t yet know how to prevent or reverse vaccine rejection.
The evidence we do have mostly tells us what not to do. Throwing more facts at sceptical parents rarely changes their minds, and often makes them more entrenched. When the MMR vaccine scare was at its height in. Within that group of decliners, only a handful are the noisy “anti-vaccination” activists.
A parent may not have thought much about vaccination and simply accepted it as ordinary. Then a bad experience with the health care system triggers mistrust, they revise their position, and begin “declining all vaccines”. It is the hesitant parents – those sitting on the fence – who are most likely to change their positions. These parents can be reassure or their concerns can be amplified. Many times, a hesitant parent will bring their concerns to a health professional who skilfully addressestheir concerns, and the parent deci.
Because these encounters are so influential and often difficult, we are investigating health professionals’ and parents’ communication needs during vaccination consultations. Health professionals have told us they need information they can give to parents about vaccination, and strategies to help them avoid arguments and reassure parents. In our recent qualitative study, parents told us they want more information about vaccination from sources they can trust, before the first appointment. This finding is also supported by other evidence, as shown in a recent review.

However, parents on the more accepting end found too much information overwhelming, reducing their confidence. Parents also want to be invited to ask questions. Ideally, governments formulate their health policies and regulations more broadly, and are concerned with the national interest. They take into account the risks to individuals, including vulnerable groups such as children. Parents, on the other han are primarily concerned with the wellbeing of their child.
Understandably, their decision is emotional and practical when they weigh up the risks of vaccination versus non-vaccination. A wealth of information on the potential side effects of vaccination is now available. Unfortunately, misinformation that instils fear about purported adverse effects can result in a decrease in coverage rates below those required to achieve herd immunity. Encouragement and incentive to vaccinate is best enshrined in. Until the late 20th century, common law assumed that a person under years of age did not have the capacity to make health decisions, including consenting to (and by default declining) medical treatment on their own behalf.
This followed with the High Court of Australia’s case Department of Health and Community Services (NT) v JWB and SMB (commonly known as ‘Marion’s case’). The two cases introduced the ‘mature minor principle’, where minors (under years of age) may be able to make healthcare decisions on their own behalf if they are assessed to be sufficiently mature and intelligent to do so. It is in this context that Australian courts would rule, in assessing the best interest of the chil whether the child refusing vaccination is ‘competent’ to make that decision.
There have been a number of cases in Australia and internationally where courts have authorised the vaccination of a child against the wishes of at least one of the parents (Box 1). In all cases, the judges ruled that they were acting in the best interest of the child and based their decision on the scientific evidence presente including risk assessments by medical practitioners. In one instance,the parents defied the New South Wales Supreme Court’s order to vaccinate and concealed the child until the period of effectiveness had lapsed. While the judge defended parens patriae – the power and authority of the state to protect persons who are unable to legally act on their own behalf – this case shows that monitoring compliance with the court’s directions can present a problem, particularly if treatments are ongoing. Parens patriaemay also empower the courts to overturn the decisions of minors who refuse treatment, no matter how ‘competent’ they are deemed to be.
Anti-vaccinationists have existed for as long as vaccines and have always agitated strongly against vaccination. Dr Sherri Tenpenny regularly delivers seminars on what she believes are the negative impacts of vaccines on health. Dr Tenpenny has warned that ‘each shot is a Russian roulette: you never know which chamber has the bullet that could kill you’.
She argues that adverse reactions listed in the package inserts include encephalitis and criticises ‘deceptive research’, claiming a shot of aluminium was used as the placebo during a safety study with the Gardasil vaccine. The anti-vaccination movement has increasingly used the internet and social media to distribute largely unchecke alarmist and misleading material. It has therefore been impossible to. Essential vaccines are provided free of charge to eligible infants, children, adolescents and adults, meeting international goals set by the World Health Organization.
Program funding agreements between governments are set up under the National Partnership Agreement on Essential Vaccines. State and territory governments are instituting more requirements to ensure children are vaccinated. The National Immunisation Program (NIP) Schedule sets out free vaccinations for children, school programs, Aboriginal and Torres Strait Islander peoples and other people at risk. The nation is aiming for a vaccination rate.
Mr Morrison said Australia also remained committed. However, government officials have said the vaccine could be. Morrison said that “there are no things that force people to do things,” adding that there will be “no compulsory vaccine, but there will be a lot of. All vaccinations carry some risk and these might be higher in the case of a quickly developed vaccine for a novel virus.
One of Australia ’s leading. But a mandatory vaccine policy can manage such risks sensibly, for instance. Three doses of the vaccine were incorporated into existing school-based vaccination programs in some jurisdictions, although in Western Australia , New. In one way or another, the three major arguments in favor of compulsory vaccination are all attempts to refute this point.
The US and Australia are among other countries where vaccinations against.