Three course modules cover. Each module will run for two (2) weeks. The development of advance care planning (ACP) skills occurs when knowledge and practice are combined. Why is advance care important?
What is advance care planning?
How to make a care plan? ACP Facilitators are instrumental in helping individuals, their families, and their loved ones become more engaged in person-centered decision making. Learn how to build support, determine goals and measures, and identify processes and standards to ensure your program is making a difference for your care recipients and your healthcare organization. Advance care planning can be a gift you give yourself and your family.
It is about doing what you can to ensure that your wishes and preferences are consistent with the health care treatment you might receive if you were unable to speak for yourself or make your own decisions. The Advance Project is a free toolkit of screening and assessment tools and a training package, designed to support nurses in Australian general practices to initiate advance care planning (ACP) and palliative care in everyday general practice. Certified Life Care Planner (CLCP) For the convenience of the reader, this certification page provides links to pages pertinent to the CLCP credential.

You will find direct access links to the CLCP application page, the CLCP examination page, and the CLCP recertification page. Please click on the appropriate menu button for the item you need. Introducing advance care planning Managers and care staff have an important role to play in supporting people to consider advance care planning , and should receive training to enable them to do so. To educate nurses on the advance care planning process, advanced directives, and the process of evaluating benefit versus burden to help patients and families make treatment choices according to their wishes and desires.
While courses use the POLST framework and provide continuing education for physicians and advanced practitioners only, course content may be useful for health professionals from all disciplines. Through small groups, role-playing with group debriefing, storytelling, and self-reflection, participants will hone their interview skills when meeting with the individual or with the. This training is for people who want to engage organizations, individuals or communities in advance care planning.
Includes CEUs for nurses, social workers and chaplains. ACP helps Medicare patients make important decisions about the type of care they get and where and when they get it. Advance Care Planning (ACP) under the Medicare Physician Fee Schedule (PFS) and the Hospital Outpatient Prospective Payment System (OPPS). Plan ahead to make sure you get the medical care you want.
Solution The Division of Supportive Care at OSF HealthCare launched OSF Care Decisions, an advance care planning (ACP) model that uses trained facilitators to help families have end-of-life care discussions. Thank you for your interest. These wishes can be expressed through several types of legal documents.
Deciding what types of treatment you would or would not want should you be diagnosed with a life-limiting illness. Sharing your personal values with your loved ones.

My sister, Dad and I worked with a nurse at VCU’s Center for Advanced Health Management, who had completed the Honoring Choices training , to do advance care planning for my dad over the summer. Lisa was great … she made a tough process very manageable. Qualified Advance Directive Facilitators. In order for someone to hold him or herself out as being a QADF, he or she must successfully complete a training program that has been approved by the Virginia Department of Health (VDH). In this course you will learn the difference between the life-cycle approach and the values-based approach.
Working with ACP Decisions has been a wonderful experience, as it has facilitated a broader and deeper understanding of what constitutes effective communication around. When someone cannot communicate, their loved ones and their health care team want to provide the best care possible. Planning in advance will help ease the transition in early retirement, financial planning , healthcare, and safety and security issues.
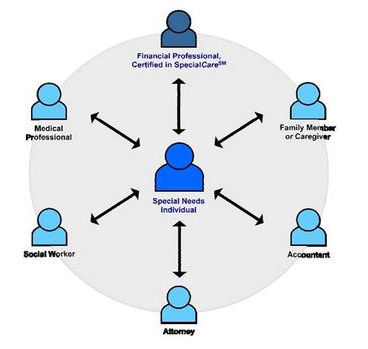
CCCC has the tools and resources to meet your needs. Our proven materials are ready to use, vetted for literacy levels, and have been demonstrated to be effective. The advance care planning (ACP) Facilitator is an emerging role in healthcare. If ACP conversations were easy, they would be more commonplace than they are today. The role of the ACP Facilitator is a critical component to achieving the ACP desired outcome—to know and honor an individual’s informed healthcare decisions.
End-of-life planning is a sensitive topic and social workers are ideally suited to initiate and guide these discussions as they explore an individual’s values and preferences. In fact, a reported percent of clinical social workers conduct advance care planning conversations (ACP) and percent are responsible for educating patients and families about ACP options. At the helm of Advance Care Training are two nursing professionals who have the knowledge and understanding of the sector to know what skills a carer needs in order to deliver high quality services. This planning process also may reduce the incidence of anxiety, depression and post-traumatic stress in surviving relatives and may improve resident and family satisfaction with care.
One of the benefits of planning in advance is that the person can participate in the decision-making process and have their wishes known.